Current and future demands of social care workers for older persons
According to population estimates and projections, the number of people aged 65 and over in England will increase by 65% from 8.2 million to 13.4 million between 2007 and 2032. Meanwhile, Malaysia is expected to become an aged nation in 2030, whereby 15% of the total population will be those aged 60 years and older, which lead to the increase in the proportion of older persons requiring care assistance. A combination of longer life expectancy (due to better health care and healthier lifestyles) especially for people with disabilities and long-term health conditions is resulting in a greater demand for social care services.
Some industries and organisations are particularly affected by the ageing population which include the care industry. The provision of care for older people relies on both the unpaid care of families and other carers alongside publicly and privately funded social care services. An ageing population and less reliance on informal care from family members due to various reasons have resulted in an increased demand for social care staff. The Size and Structure of the Adult Social Care Sector and Workforce in England 2014 report estimates that the number of paid adult social care jobs in 2025 could increase from the current 1.52 million to between 1.82 and 2.34 million; this is an increase of between 20% and 54% in a relatively short time period. In addition to the number of new workers required to keep up with the increasing demand, the care sector has other issues such as high vacancy rates and staff retention. This stretches the numbers of workers required, to keep up with demand, even further.
UK
The provision of social care in England, Scotland and Wales is split geographically into regions known as local authorities (England and Wales) or unitary authorities (Scotland). There are 152 of these authorities (councils) in England that have responsibilities for adult social care services, 32 in Scotland, and 22 in Wales [1]. Social care is provided separately to health care in England, Scotland and Wales. In some instances, funding for health and social care may be pooled (“pooled budgets”) to buy integrated health and social care services for adults. In Northern Ireland, health and social care are integrated, where services are commissioned and provided through five trusts.
Social care offered to adults in England is subject to rules about eligibility – that is, whether or not a person’s needs are assessed to be severe enough to receive care. Local authorities use a set of national criteria to assess an individual’s needs (these national criteria are summarised by Age UK here).
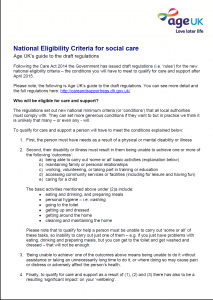
Criteria are based on whether or not an individual can achieve certain outcomes (e.g. around activities of daily living) and whether or not there is an impact on well-being if unable to achieve such outcomes. Individuals are only eligible for care if they have very high needs – that is, they have a lot of difficulty with at least two of the outcomes listed. Many will not be considered eligible for care [2]. For example, in the financial year 2015/2016, there were 1,811,000 new requests for support, of which 57% resulted in no ‘direct’ support from the council. [3] If an individual is not eligible for care under the national criteria, they can arrange and pay for their own care through private providers.
It is estimated that the labour market of adult social care in England comprises 1,550,000 jobs. The largest proportion (78%) of these were located within independent organisations (i.e. services provided by the private and voluntary sector), with just 8% located within local authorities. Similarly small proportions of adult social care jobs were also located within the National Health Service (6%) and for staff employed independently by those organising their own care through the receipt of direct payments (8%). Of those receiving direct payments, around 28% are estimated to be employing care staff [4]. The adult social care workforce in England largely consists of care workers (73%), followed by managerial staff (9%), social workers, occupational therapists and nurses (6%), and other roles such as administrative staff (13%) [5].
Malaysia
In Malaysia the social care sector is mainly managed by the government which is organised by the Department of Social Welfare Malaysia (DSWM) under the provision of Ministry of Women, Family and Community Development. The social care facilities and service for older people provided by government, and non-governmental, charitable and religious organisations. There are three categories of residential care (1) Public residential homes which are directly under DSWM under the Ministry of Women, Family and Community Development (2) Private residential homes managed by voluntary organization and private agencies which are profits driven and, (3) Religious homes which are privately owned and mainly derived from religious pursuit.
The amount of money spent by the Department of Social Welfare on the welfare of the Malaysian elderly in 2015 was approximately RM 6 billion, which is expected to increase to RM 33 billion in 2030. The long-term care for older people provided by DSWM consists of ten residential homes for independent elderly which is also known as Rumah Seri Kenangan (RSK) and two public nursing homes for critically ill or bedridden elderly, known as Rumah Ehsan (RE). Apart from the residential homes, the Department of Social Welfare funds the non-residential type of social care, known as the daily activity centre (Pusat Aktiviti Warga Emas, PAWE) and home help services which directly supervised by DSWM. The daily activity centres are currently operated and managed by the elderly representatives in the community and the home help services are run based on volunteerism nature in providing domiciliary type of social care for older persons in need.
Although increasing demands towards the social care services are seen, independent or semi-dependent older persons should be encouraged to stay in their own house and the presence of social care workers should be limited to minimally assist them conducting their activity of daily living at their own place. This is parallel to the ageing in place initiative that has been promoted by the World Health Organization (WHO).
One of the managers of an elderly care home that was interviewed for the project emphasised on the role of the centre for “rehabilitation and neutralisation” and continuation of normal living in the community once satisfactory recovery process is achieved. Effort should be given towards the provision of domiciliary care, a type of aged care that has been widely and aggressively implemented in many developed countries including England. The voluntary approach that was adopted by the Department of Social Welfare Malaysia in the implementation of the Home Help Program should be revised and switched to a more effective strategy. However, older persons who are fully dependent with no family members are better served and managed in the institutional care that integrates both medical and social care services. With the majority of the older persons in Malaysia are considerably cash poor, the government should also find a future alternative pathway such as the long term care insurance, in order to increase the accessibility of the in need older persons towards the care services which can be very expensive depending on the level of care needed.
- Ham, C., et al., Integrated care in Northern Ireland, Scotland and Wales. 2013, King’s Fund: London.
- Reade, N (2015). The Suprising Truth About Older Workers. AARP The Magazine. Available at https://www.aarp.org/work/job-hunting/info-07-2013/older-workers-more-valuable.html
- Reynolds, F. A., Farrow, A., Blank, A. (2012). ‘Otherwise it would be nothing but cruises’: Exploring the subjective benefits of working beyond 65. IJAL. 7(1):79–106. doi: 10.3384/ijal.1652-8670.127179.
- Sewdas, R., de Wind, A., van der Zwaan, L. G., van der Borg, W. E., Steenbeek, R., van der Beek, A. J., & Boot, C. R. (2017). Why older workers work beyond the retirement age: a qualitative study. BMC public health, 17(1), 672.








